Lung cancer is a disease characterized by uncontrolled cell growth in tissues of the lung. If left untreated, this growth can spread beyond the lung in a process called metastasis into nearby tissue and, eventually, into other parts of the body. Most cancers that start in lung, known as primary lung cancers, are carcinomas that derive from epithelial cells. The main types of lung cancer are small-cell lung carcinoma (SCLC), also called oat cell cancer, and non-small-cell lung carcinoma (NSCLC). The most common cause of lung cancer is long-term exposure totobacco smoke,[1] which causes 80–90% of lung cancers.[2] Nonsmokers account for 10–15% of lung cancer cases,[3] and these cases are often attributed to a combination of genetic factors,[4] radon gas,[4] asbestos,[5] and air pollution[4] including secondhand smoke.[6][7]
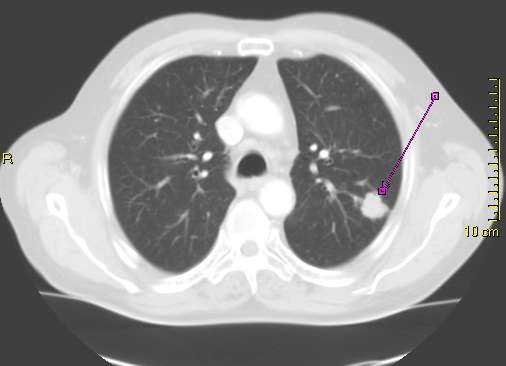

The most common symptoms are coughing (including coughing up blood), weight loss and shortness of breath.[2] Lung cancer may be seen on chest radiograph and computed tomography (CT scan). The diagnosis is confirmed with a biopsy.[8] This is usually performed by bronchoscopy or CT-guided biopsy. Treatment and prognosis depend on the histological type of cancer, the stage (degree of spread), and the patient's general well-being, measured by performance status. Common treatments include surgery, chemotherapy, and radiotherapy. NSCLC is sometimes treated with surgery, whereas SCLC usually responds better to chemotherapy and radiotherapy.[9]
Survival depends on stage, overall health, and other factors. Overall, 15% of people in the United States diagnosed with lung cancer survive five years after the diagnosis.[10] Worldwide, lung cancer is the most common cause of cancer-related death in men and women, and is responsible for1.38 million deaths annually, as of 2008.[11]
Signs and symptoms
Symptoms and signs that may suggest lung cancer include:[2]
respiratory symptoms: coughing, hemoptysis (coughing up blood), wheezing or dyspnea (shortness of breath)
systemic symptoms: weight loss, fever, clubbing of the fingernails, or fatigue
symptom due to local compress: chest pain, bone pain, superior vena cava obstruction, dysphagia (difficulty swallowing)
If the cancer grows in the airway, it may obstruct airflow, causing breathing difficulties. The obstruction can lead to accumulation of secretions behind the blockage, and predispose to pneumonia.[2]
Depending on the type of tumor, so-called paraneoplastic phenomena may initially attract attention to the disease.[12] In lung cancer, these phenomena may include Lambert–Eaton myasthenic syndrome (muscle weakness due to autoantibodies), hypercalcemia, or syndrome of inappropriate antidiuretic hormone (SIADH). Tumors in the top (apex) of the lung, known as Pancoast tumors, may invade the local part of the sympathetic nervous system, leading to Horner's syndrome, as well as damage to the brachial plexus.[2]
Many of the symptoms of lung cancer (poor appetite, weight loss, fever, fatigue) are not specific.[8] In many patients, the cancer has already spread beyond the original site by the time they have symptoms and seek medical attention. Common sites of metastasis include the brain, bone,adrenal glands, contralateral (opposite) lung, liver, pericardium, and kidneys.[13] About 10% of people with lung cancer do not have symptoms at diagnosis; these cancers are incidentally found on routine chest radiograph.[10]
Causes
Cancer develops following genetic damage to DNA. This genetic damage affects the normal functions of the cell, including cell proliferation, programmed cell death (apoptosis) and DNA repair. As more damage accumulates, the risk of cancer increases.[14]
Smoking
NIH graph showing how a general increase in sales of tobacco products in the USA in the first four decades of the 20th century (cigarettes per person per year) led to a corresponding rapid increase in the incidence of lung cancer during the 1930s, '40s and '50s (lung cancer deaths per 100,000 male population per year)
Cross section of a human lung: The white area in the upper lobe is cancer; the black areas are discoloration due tosmoking.
Smoking, particularly of cigarettes, is by far the main contributor to lung cancer.[15] Cigarette smoke contains over 60 known carcinogens,[16] including radioisotopes from the radon decay sequence, nitrosamine, and benzopyrene. Additionally, nicotine appears to depress the immune response to malignant growths in exposed tissue.[17] Across the developed world, 90% of lung cancer deaths in men during the year 2000 were attributed to smoking (70% for women).[18] Smoking accounts for 80–90% of lung cancer cases.[2]
Passive smoking—the inhalation of smoke from another's smoking—is a cause of lung cancer in nonsmokers. A passive smoker can be classified as someone living or working with a smoker. Studies from the US,[19][20] Europe,[21] the UK,[22] and Australia[23] have consistently shown a significantly increased risk among those exposed to passive smoke.[24] Those who live with someone who smokes have a 20–30% increase in risk while those who work in an environment with second hand smoke have a 16–19% increase in risk.[25] Investigations of sidestream smoke suggest it is more dangerous than direct smoke.[26] Passive smoking causes about 3,400 deaths from lung cancer each year in the USA.[20]
Radon gas
Radon is a colorless and odorless gas generated by the breakdown of radioactive radium, which in turn is the decay product of uranium, found in the Earth's crust. The radiation decay products ionize genetic material, causing mutations that sometimes turn cancerous. Radon is the second-most common cause of lung cancer in the USA, after smoking.[20] The risk increases 8–16% for every 100 Bq/m³ increase in the radon concentration.[27] Radon gas levels vary by locality and the composition of the underlying soil and rocks. For example, in areas such as Cornwall in the UK (which has granite as substrata), radon gas is a major problem, and buildings have to be force-ventilated with fans to lower radon gas concentrations. The United States Environmental Protection Agency (EPA) estimates one in 15 homes in the US has radon levels above the recommended guideline of 4 picocuries per liter (pCi/l) (148 Bq/m³).[28]
Asbestos
Asbestos can cause a variety of lung diseases, including lung cancer. Tobacco smoking and asbestos have a synergistic effect on the formation of lung cancer.[5] Asbestos can also cause cancer of the pleura, called mesothelioma (which is different from lung cancer).[29]
Air pollution
Outdoor air pollution has a small effect on increasing the risk of lung cancer.[4] Fine particulates (PM2.5) and sulfate aerosols, which may be released in traffic exhaust fumes, are associated with slightly increased risk.[4][30] For nitrogen dioxide, an incremental increase of 10 parts per billion increases the risk of lung cancer by 14%.[31] Outdoor air pollution is estimated to account for 1–2% of lung cancers.[4]
Genetics
Some people have a genetic predisposition to lung cancer. In relatives of people with lung cancer, the risk is increased 2.4 times. This may be due to genetic polymorphisms.[32]
Other causes
Numerous other substances, occupations, and environmental exposures have been linked to the genesis of cancer in lung tissue of humans. The International Agency for Research on Cancer (IARC) states there is "sufficient evidence" to show the following are carcinogenic in lung:[33]
-Some metals (Aluminum production, Cadmium and cadmium compounds, Chromium(VI) compounds, Beryllium and beryllium compounds, Iron and steel founding, Nickel compounds, Arsenic and inorganic arsenic compounds, Hematite mining (underground))
-Some products of combustion (incomplete combustion, Coal (indoor emissions from household coal burning), Coal gasification, Coal-tar pitch, Coke production, Soot, Diesel engine exhaust)
-Ionizing radiation (X-radiation, Radon-222 and its decay products, Gamma radiation, Plutonium)
-Some toxic gases (Methyl ether (technical grade), Bis-(chloromethyl) ether, Sulfur mustard, MOPP (vincristine-prednisone-nitrogen mustard-procarbazine mixture), fumes from painting)
-Rubber production industry
-Silica dust (crystalline)
Pathogenesis
See also: Carcinogenesis
Similar to many other cancers, lung cancer is initiated by activation of oncogenes or inactivation of tumor suppressor genes.[34] Oncogenes are believed to make people more susceptible to cancer. Proto-oncogenes are believed to turn into oncogenes when exposed to particular carcinogens.[35] Mutations in the K-ras proto-oncogene are responsible for 10–30% of lung adenocarcinomas.[36][37] The epidermal growth factor receptor (EGFR) regulates cell proliferation, apoptosis, angiogenesis, and tumor invasion.[36] Mutations and amplification of EGFR are common in non-small-cell lung cancer and provide the basis for treatment with EGFR-inhibitors. Her2/neu is affected less frequently.[36] Chromosomal damage can lead to loss of heterozygosity. This can cause inactivation of tumor suppressor genes. Damage to chromosomes 3p, 5q, 13q, and 17p are particularly common in small-cell lung carcinoma. The p53 tumor suppressor gene, located on chromosome 17p, is affected in 60-75% of cases.[38] Other genes that are often mutated or amplified are c-MET, NKX2-1, LKB1, PIK3CA, and BRAF.[36]
Prevention
See also: Smoking ban
Prevention is the most cost-effective means of mitigating lung cancer development. While in most countries, industrial and domestic carcinogens have been identified and banned, tobacco smoking is still widespread. Eliminating tobacco smoking is a primary goal in the prevention of lung cancer, and smoking cessation is an important preventive tool in this process.[48]
Policy interventions to decrease passive smoking in public areas such as restaurants and workplaces have become more common in many Western countries.[49] Bhutan has had a complete smoking ban since 2005.[50] India introduced a ban on smoking in public in October 2008.[51]
The World Health Organization has called for governments to institute a total ban on tobacco advertising to prevent young people from taking up smoking. They assess that such bans have reduced tobacco consumption by 16% where instituted.[52]
The long-term use of supplemental vitamin A,[53][54] vitamin C,[53] vitamin D[55] or vitamin E[53] does not reduce the risk of lung cancer. Some studies suggest people who eat diets with a higher proportion of vegetables and fruit tend have a lower risk,[20][56] but this is likely due toconfounding. More rigorous studies have not demonstrated a clear association.[56]
Screening
Main article: Lung cancer screening
Screening refers to the use of medical tests to detect disease in asymptomatic people. Possible screening tests for lung cancer include sputum cytology, chest radiograph (CXR), and computed tomography (CT). Screening programs using CXR or cytology have not demonstrated any benefit.[57] Screening those at high risk (i.e. age 55 to 79 who have smoked more than 30 pack years or those who have had previous lung cancer) annually with low-dose CT scans may reduce the chance of death from lung cancer by an absolute amount of 0.3% (relative amount of 20%).[58][59]The potential risks of screening however are not well known.[60]