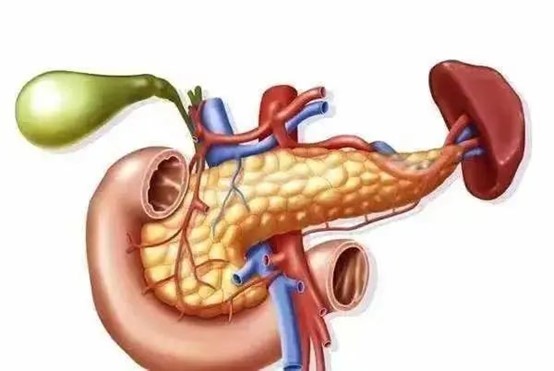
In daily life, people who frequently binge eat and drink heavily are prone to developing pancreatitis. Pancreatitis is an inflammatory reaction caused by the activation of pancreatic enzymes within the pancreas, leading to the pancreas digesting its own tissues, resulting in edema, hemorrhage, and even necrosis.
Clinically, pancreatitis is classified into acute and chronic forms, with acute pancreatitis being a surgical emergency characterized by a sudden onset and severe course. If it progresses to severe acute pancreatitis, treatment becomes more challenging, and it can lead to multiple organ failure with a high mortality rate. Recently, Dr. Long Xin'an from the First Department of Medicine at Guangzhou Fuda Cancer Hospital shared the latest research on the diagnosis and treatment of acute pancreatitis.
What is Acute Pancreatitis?
Acute pancreatitis (AP) refers to a sudden abdominal condition characterized by local inflammation of the pancreas due to the abnormal activation of pancreatic enzymes, which digest the pancreas and surrounding organs. Approximately 20% of patients may develop severe acute pancreatitis (SAP), which progresses rapidly and has a poor prognosis, often accompanied by pancreatic or peripancreatic tissue necrosis or organ failure, with a mortality rate of 20% to 40%. Therefore, it is crucial to accurately distinguish between the different types of acute pancreatitis.
How is Acute Pancreatitis Diagnosed?
Persistent upper abdominal pain.
Serum amylase and/or lipase concentrations at least three times the upper limit of normal.
Imaging studies showing changes consistent with acute pancreatitis.
A diagnosis of acute pancreatitis can be made if two of the above three criteria are met. When clinical symptoms or laboratory results are uncertain, imaging studies help confirm the diagnosis.
Ultrasound: Limited in diagnosing acute pancreatitis and its complications, but useful for assessing biliary dilation or stones. Early identification of bile duct stones is important for prognosis. Ultrasound should be performed within 48 hours of admission for patients suspected of having biliary pancreatitis.
CT Imaging: Typical CT features do not reflect disease severity, but contrast-enhanced CT accurately indicates the presence and extent of pancreatic necrosis. The best time for the first enhanced CT assessment is 72-96 hours after onset. The Modified CT Severity Index (MCTSI) helps assess the severity of acute pancreatitis. It is important to note that contrast-enhanced CT is not recommended early in the disease unless necessary for diagnosis.
MRI: Suitable for patients allergic to iodinated contrast agents, those with renal insufficiency, or young/pregnant patients. Magnetic resonance cholangiopancreatography (MRCP) or endoscopic ultrasound (EUS) can help detect occult biliary stones.
How is the Severity of Acute Pancreatitis Classified?
The Revised Atlanta Classification (RAC) and Determinant-Based Classification (DBC) are commonly used to classify the severity of acute pancreatitis, with RAC being more prevalent. There is no significant difference between the two in predicting mortality, ICU admission rates, or ICU length of stay.
Organ Dysfunction Diagnosis: Based on the Modified Marshall Scoring System, organ dysfunction is defined as any organ score ≥2.
How is Acute Pancreatitis Treated?
Early Treatment:
Fluid Therapy: Recommended at a rate of 5-10 mL/kg/h, with caution to avoid fluid overload.
Pain Management: An important supportive treatment that may improve patient outcomes. Pain relief should be tailored to the patient's condition.
Nutritional Therapy: Early enteral nutrition within 24-48 hours is supported by multiple meta-analyses, leading to lower infection and organ dysfunction rates. Nasogastric tube feeding is recommended for patients with delayed gastric emptying or pyloric obstruction.
Early Treatment of Hyperlipidemic Acute Pancreatitis: Combined treatment methods should be used to rapidly lower triglyceride levels, with a target of <5.65 mmol/L.
Early Management of Abdominal Compartment Syndrome (ACS): Involves comprehensive measures to reduce intra-abdominal pressure.
Antibiotics: Routine use of antibiotics for the prevention of pancreatic or peripancreatic infection is not recommended.
Medication: There is a lack of high-quality clinical evidence supporting the use of protease inhibitors or enzyme inhibitors, such as somatostatin and its analogs, in the treatment of acute pancreatitis.
Later Treatment:
Infected Pancreatic Necrosis (IPN): When symptoms of infection appear, IPN should be considered. The first-line intervention strategy is the "Step-up" approach, starting with puncture drainage and progressing to more invasive procedures if necessary.
Indications and Timing of PCD and Endoscopic Puncture Drainage: Pancreatic or peripancreatic infection is a major indication for PCD and endoscopic puncture drainage, which may be performed early in the disease course.
Pancreatic Fistula and Disconnected Pancreatic Duct Syndrome (DPDS): Endoscopic treatment is the first choice.
Pancreatic Pseudocyst (PPC): Infected PPCs often require drainage or surgery.
Follow-Up: Patients should be regularly followed up to monitor pancreatic exocrine and endocrine function, with specific attention to long-term complications and recurrence prevention.