"Your thyroid nodules on both sides tested malignant in the biopsy, and there is lymph node metastasis in the neck. In this case, ablation is not suitable — surgery should be the primary treatment."
I once encountered a patient with thyroid nodules who specifically came to seek ablation therapy. However, in general, ablation is more appropriate for nodules less than 1 cm in size, with no lymph node metastasis, and classified as low-risk thyroid cancer pathologically. Clearly, this patient's condition was unsuitable for ablation. I declined her request, and eventually, Professor Zeng Zongyuan, a head and neck oncology expert from our hospital, performed surgery on her. She is currently recovering well.

△ Communicating with the patient


△ This patient also had thyroid cancer with lymph node metastasis. Surgical resection was the first choice, and one of the keys to a successful surgery was thorough lymph node dissection.
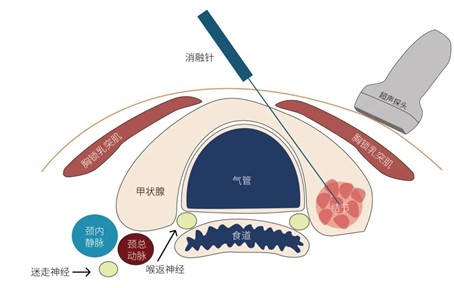
Thermal ablation of thyroid nodules is a minimally invasive technique that includes radiofrequency ablation (RFA), microwave ablation (MWA), and laser ablation (LA). Under real-time ultrasound guidance, an ablation needle is precisely inserted percutaneously into the thyroid nodule. Once the device is activated, the electrode generates heat, causing the water content in the diseased tissue to evaporate, dry, coagulate, and necrotize, eventually being naturally absorbed by the body, thus achieving therapeutic effects.
This technology has been applied for over 20 years both domestically and internationally. It offers advantages such as minimal invasiveness, good repeatability, fast recovery, preservation of thyroid function, and favorable cosmetic outcomes, making it more acceptable to patients.
For benign thyroid nodules, thermal ablation has gradually become an alternative to surgical excision and has shown satisfactory results. For instance:
In 2020, the European Thyroid Association (ETA) published the Guidelines for Image-Guided Ablation of Benign Thyroid Nodules, clearly stating that thermal ablation is an effective treatment for symptomatic benign thyroid nodules. Laser ablation and radiofrequency ablation were recommended as first-line options, while microwave ablation, rarely used in Europe, was listed as a second-line choice.
In 2022, the American Head and Neck Society-Endocrine Section and the European Thyroid Association jointly issued an International Multidisciplinary Expert Consensus Statement on the use of RFA and related ultrasound-guided ablation techniques for benign and malignant thyroid diseases. It clearly pointed out that for benign thyroid nodules causing compressive symptoms or cosmetic concerns, ultrasound-guided thermal ablation can be considered a first-line alternative to surgery. For patients with autonomously functioning thyroid nodules who have contraindications to first-line treatments, thermal ablation offers a safe alternative.
However, when it comes to thermal ablation for thyroid cancer, opinions among scholars remain divided. For example:
In 2024, the Tumor Ablation Therapy Professional Committee of the China Anti-Cancer Association released the Expert Consensus on Thermal Ablation for Papillary Thyroid Carcinoma. Some of its recommendations sparked widespread debate. The consensus recommended "thermal ablation as one of the first-line treatments for T1aN0M0 PTC (papillary thyroid carcinoma)" (strong recommendation, high-quality evidence).
Some scholars argue that the cited evidence in the consensus lacked randomized controlled trials comparing thermal ablation with conservative management. Furthermore, while the evidence focused on carefully selected low-risk, solitary T1aN0M0 tumors, the consensus extended the recommendation to broader cases, including T1b tumors and multifocal or clinically higher-risk PTCs.
Additionally, they pointed out that the studies cited had relatively short follow-up durations — with a maximum of only 34.57 months — which is insufficient given the generally slow progression of PTC.
Similarly, in the 2024 Draft Guidelines for Adult Differentiated Thyroid Cancer recently released by the American Thyroid Association (ATA), thermal ablation was not included as a routine initial treatment for differentiated thyroid cancer.
In Korea, the guidelines for RFA in recurrent thyroid cancer were updated on January 2, 2025, after nearly seven years. While acknowledging the growing body of evidence for thermal ablation, the guidelines emphasize that it should be reserved for patients who refuse surgery or for whom surgery poses high risks.
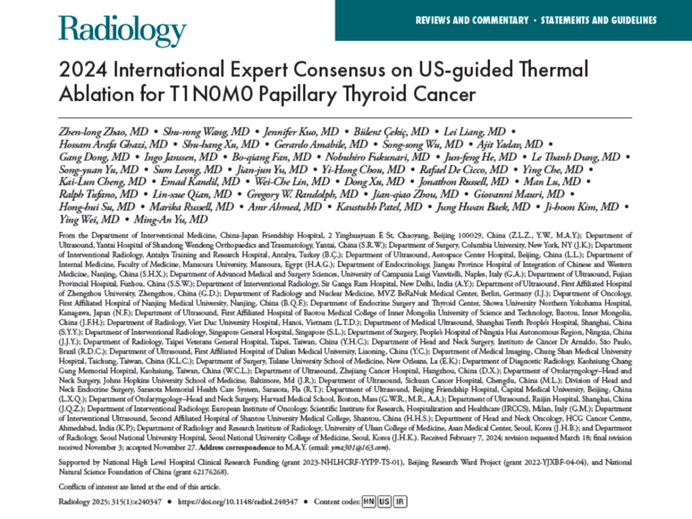
It is worth noting that in April 2025, the First International Expert Consensus on Thermal Ablation for T1N0M0 Papillary Thyroid Carcinoma was published in Radiology, a leading international medical journal.
This consensus marked a major breakthrough: for the first time, it expanded the indications for thermal ablation beyond T1a (tumor diameter <1 cm) to include T1b (tumor diameter <2 cm) papillary thyroid carcinomas, multifocal tumors, microcapsular invasion, and tumors located in the thyroid isthmus. It also elevated thermal ablation to the same status as surgery as a first-line treatment option.
This signifies that thermal ablation for T1-stage papillary thyroid carcinoma has gained international recognition from experts.
Currently, there is still significant debate and discussion on this topic, largely due to disciplinary differences. Thermal ablation technology is now highly mature, with its safety and efficacy well established.
What’s crucial is to clearly define its indications and the appropriate timing for its use — selecting technology based on the patient's condition, rather than selecting patients based on the available technology.